I hope you're doing well and enjoying spring. I also hope you'll find the following article about
controlling indoor allergens by Dr. Harriet Burge both interesting and useful.
With best wishes,
Dave Gallup
Controlling Indoor Allergens
By Dr. Harriet Burge, EMLab P&K Chief Aerobiologist and Director of Scientific Advisory Board
"Indoor allergens" is a term coined by allergists to include allergens produced
by dust mite, cockroach, mouse, rat, pet dander and mold (Diette et al. 2008). It is a useful
term because exposure to most of these allergens occurs indoors. While mold fungi clearly can
grow indoors, most exposure occurs outdoors, so they will not be included here.
There are two general approaches to the control of indoor allergens. One can attempt to control
the sources (e.g., the dust mites, cats, cockroaches, etc.), or one can attempt to remove the
allergens (e.g., the actual proteins that cause sensitization). Which of these two methods is
preferred depends on the allergen source.
It is also important to note that the development of allergies is a complex process involving
genetics and the environment. While environmental control can reduce symptoms in allergic
individuals, there is conflicting evidence as to whether or not environmental control reduces
the risk of developing allergies in susceptible individuals (Bush 2008).
Dust Mites
The study of indoor allergens began when the dust mite allergen was discovered. Before that
time, patients with indoor symptoms were skin tested with extracts of house dust, usually
from some standard source other than their own environment. Those that tested positive were
considered "house dust" sensitive. Patients with house dust sensitivity were
given a regimen to render their home "dust free." This included:
- Remove all carpeting.
- Use only washable drapes and comforters.
- Minimize the use of upholstered furniture.
- Remove all dust catchers (knick knacks, books, etc.).
- Vacuum regularly with the sensitive person not doing the vacuuming.
The allergen control procedures described above are still advised today. However, a group
of Dutch researchers, after long and persistent effort, identified the house dust mite as
the source for house dust allergens (Dieges 2004). With that discovery, there was a specific
target for remediation efforts and the study of the house dust mite intensified. Research
revealed that the dust mite did not drink water, but absorbed it from the air (Arlian &
Morgan 2003). The dust mite needed a place to live where both humidity and temperature remained
high. Bedding turned out to be the ideal "nest" for these organisms.

Figure 1: Magnified photograph of a house dust mite.
Source: U.S. Food and Drug Administration
The requirement for high humidity indicated that lowering humidity could possibly control
dust mite populations. Also, using barriers to prevent entry of dust mites into bedding
could possibly prevent exposure. A number of studies confirmed both of these hypotheses
and also the fact that washing bedding in hot water would kill dust mites and remove the
allergen. Thus the industry of mattress and pillow encasings developed, and allergy
sufferers returned to the hot water cycle of their washing machines. Lowering humidity
was a more difficult problem. In occupied beds the humidity is inevitably high due to
respiration (which yields CO2 and H20). Fortunately, the encasings
and hot water washes were generally sufficient to control populations. The fact remains
that the dust mites can also "nest" in carpeting and upholstered furniture
providing the humidity is high. In the very humid parts of the world the only practical
solution is to follow the early advice to remove carpets and upholstered furniture. If
humidity is only high part of the year (as in the Northeastern U.S.), rugs can be used
in the winter and stored in the summer. Our great grandparents did this and so can we.
In very dry climates dust mites are much less of a problem and avoiding the addition of
water to interior spaces will generally control their populations.
Chemical treatments have been studied for the reduction of dust mite allergens in
carpeting. Benzyl Benzoate, 3% tannic acid spray and two carpet cleaners successfully
reduced dust mite allergen concentrations in carpeting for approximately 2 weeks.
Treatments were not effective for cat allergen. Other types of chemical treatment have
not been sufficiently tested to warrant recommendation. Washing bedding in hot water
continues to be recommended for control of dust mite allergen, although controlled
trials have not been done to evaluate efficacy at preventing symptoms.
Cockroaches
Cockroaches were first linked to allergic disease in 1964 by Bernton and Brown.
Of the 43% of the U.S. population that is allergic to at least one common indoor
allergen, 26% are sensitive to German cockroaches (Blattella germanica). Allergens
from the German cockroach and the American cockroach (Periplanata americana) have
been isolated and are officially recognized.
The German cockroach colonizes the built environment, especially where food is prepared.
German cockroach infestation is most common in the Northeastern U.S. The American
cockroach generally lives outdoors or in sewers, but can also be found as the dominant
indoor roach in tropical regions. Cockroaches have long been thought to carry infectious
diseases, and some pathogens can be found on their bodies. However, there are no
documented cases of any infection directly transferred from cockroaches to people.
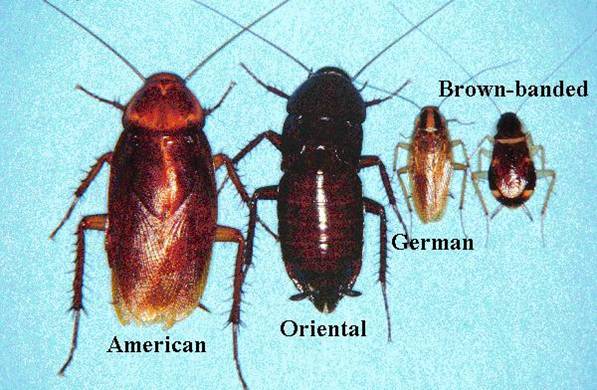
Figure 2:
Cockroach species that commonly inhabit human dwellings include the following:
German cockroach (Blattella germanica); American cockroach (Periplaneta americana);
Oriental cockroach (Blatta orientalis); brown-banded cockroach (Supella longipalpa);
Australian cockroach (Periplaneta australasiae); smoky-brown cockroach (Periplaneta
fuliginosa); and brown cockroach (Periplaneta brunnea).
Source: Centers for Disease Control and Prevention
Exposure to cockroach allergens clearly leads to both sensitization and symptoms of asthma
(Chew et al. 2008). Guidelines for exposure leading to sensitization, (2-4 Units Bla g 1
per gram of vacuumed, sieved house dust), and symptoms, (8 Units Bla g 1 per gram),
have been suggested.
As for other indoor allergens, two approaches to exposure reduction may be employed.
Cockroach populations can be suppressed, and the allergens may be removed by cleaning.
Studies show that without cockroach suppression, cleaning is not an effective means for
significantly reducing allergen loads. However, pest control alone can be effective.
Studies evaluating the efficacy of commercial pest management were disappointing (Sever
et al. 2007). However, research entomologists were able to achieve significant population
reductions. The steps they used are as follows:
- 18 cockroach traps placed throughout the home for 1 week.
- Bait applications applied with amounts depending on number of cockroaches at each trap site.
- Bait used: 2.15% Hydramethylnon (Maxforce Roach Killer Gel Bait; Bayer Environmental Science, Research Triangle Park, NC).
- Baits placed: months 0, 1, 3, 6, and 9 in areas where traps had cockroaches.
- New traps placed at each visit.
So, to put this into practical terms: Each home must be entered first to place traps, then
a week later to place bait. Traps are placed where cockroaches are most likely to be. Bait
is applied wherever there are cockroaches in the traps. Each time new bait is applied, new
traps are laid. This process is continued approximately monthly until no more cockroaches
appear in the traps.
Rodent Pests
Rodent infestation is common. More than 50% of randomly selected U.S. homes had detectable
mouse allergen (Cohn et al. 2004) and prevalence was even higher in the inner city,
especially in detached homes (Berg et al. 2007). Asthma is an epidemic in the inner city,
and sensitization to rodent allergens is a risk factor for having asthma (Donahue et al. 2008).
Rodent allergens are also common in classrooms.
Integrated pest management is required to reduce infestations with rodents. This includes
application of pesticides, plugging access to the indoors, and preventing access to any food.
The latter includes storing dry foodstuffs in sealed metal containers. Thorough, vigorous,
and frequent cleaning to remove residual allergens must follow pest management. Even with
intensive management and cleaning, rodent allergen was shown to only fall by about 42% in
one study (Eggleston 2005).

Figure 3: Mouse and rodent allergens are common in houses and classrooms.
Source: U.S. Department of Housing and Urban Development
Cats
Cat allergen is a conundrum. Individuals do become sensitive to cat allergen, and develop
asthma as a result. However, in epidemiological studies, concentrations of cat allergen
are correlated with a decreased risk of asthma (Takkouche et al. 2008).
Cat allergen cannot be completely removed. A cleaning protocol that included vacuuming,
dry mopping, then wet mopping and shaking pillows and small rugs outdoors reduced dust
levels and, to a small extent, cat allergen concentrations (Adgate et al. 2008). The
type of carpet apparently does not affect the ease of removing cat allergen, but allergen
can be removed more easily from new rather than from old carpets (Causer et al. 2008).
High efficiency filtration in a central forced air system was found to remove up to 55%
of airborne cat allergen.
Removal of the pet cat will eventually lead to allergen reduction after 4-6 months.
Thorough cleaning and dust removal will speed this along. Room air cleaning is not an
efficient method for removing exposure (Diette et al. 2008), nor is washing the pet or
isolating the pet from the bedroom (Eggleston 2005).
Dogs
Sensitization to dog allergen is strongly associated with asthma (Korppi et al. 2008).
As with cat allergies, early exposure to dogs may lessen the risk of sensitization and subsequent
asthma development. However, this effect, while seen in univariate analyses, disappears
when multivariate techniques are used.
Removal of dog allergen is similar to that described for cat allergen. Dogs can survive
as primarily outdoor animals, whereas the average life span for an outdoor cat is only
about 2 years.
Other Indoor Allergen Sources
Almost any animal, fungus or plant can release allergens into the indoor environment.
In order to decide on a remediation protocol, the nature of the source and the dynamics
of allergen dispersal need to be considered. For mammals, allergen is generally contained
in skin secretions, saliva, and/or urine. For arthropods, feces and eggs may contain the
allergen, or secretions may be at fault. For many plants, the majority of allergens are
contained in pollen. In each of these cases, exposure prevention involves removing the
source, or somehow blocking the pathway of the allergen. In domestic environments,
removal of sources is by far the best approach to reducing allergen exposure.
References:
Adgate JL, Curumurthy R, Sook JAC, Ryan AD, Grengs J. Allergen levels in inner city homes:
baseline concentrations and evaluation of intervention effectiveness. Journal of Exposure
Science and Environmental Epidemiology 2008. 18:430-440
Arlian LG, Morgan MS. Biology, ecology, and prevalence of dust mites. Immunol Allergy
Clin N Am 2003. 23:443-468
Berg J, McConnell R, Milam J, Galvan J, Kotlerman J, Thorne P, Jones C, Ferdman R,
Eggleston P, Rand C, Lewis MA, Peters J, Richardson J. Rodent allergen in Los Angeles inner
city homes of children with asthma. Journal of Urban Health: Bulletin of the New York Academy
of Medicine 2007. 85(1):52-61
Bernton HS, Brown H. Insect allergy, preliminary studies of the cockroach. J. Allergy 1964. 35:506
Bush RK. Indoor allergens, environmental avoidance, and allergic respiratory disease. Allergy
Asthma Proc 2008. 29:575-579
Causer SM, Shorter CL, Lewis RD, Siebers RW. Carpets of different construction efficiency of
vacuuming for the removal of cat allergen (Fel d 1) from worn and unworn wool. Textile Research
Journal 2008. 78:105
Chew GL, Perzanowski MS, Canfield SM, Goldstein IF, Mellins RB, Hoepner LA, Ashby-Thompson M,
Jacobson JS. Cockroach allergen levels and associations with cockroach-specific IgE. J Allergy
Clin Immunol 2008. 121(1): 240-245
Cohn RD, Arbes SJ Jr, Yin M, Jaramillo R, Zeldin DC. National prevalence and exposure
risk for mouse allergen in US households. J Allergy Clin Immunol 2004. 113(6):1167-1171
Dieges PH. The history of the finding of the house dust mite. J Allergy Clin Immunol. Allergy
Archives 2004. 113(3):573-576
Diette GB, McCormack MC, Hansel NN, Breysse PN, Matsui EC. Environmental issues in managing
asthma. Respiratory Care 2008. 53(5):602-617
Donohue KM, Al-alem U, Perzanowski MS, Chew GL. Anti-cockroach and antimouse IgE are associated
with early wheeze and atopy in an inner-city birth cohort. J Allergy Clin Immunol 2008. 122(5): 914-920
Eggleston PA. Improving indoor environments: reducing allergen exposures. J Allergy Clin Immunol 2005. 116(1): 122-126
Korppi M, Hyvarinen M, Kotaniemi-Syrjanen A, Piippo-Savolainen E, Reijonen T. Early
exposure-sensitization to cat and dog: different effects on asthma risk after wheezing in
infancy. Pediatric allergy and Immunology 2008. 19(8):696-701
Sever ML, Arbes SJ Jr, Gore JC, Santangelo RG, Vaughn B, Mitchell H, Schal C, Zeldin DC.
Cockroach allergen reduction by cockroach control alone in low-income urban homes: a
randomized control trial. J Allergy Clin Immunol 2007. 120(4):849-855
Takkouche B, GonzÁlez-Barcala F-J, Etminan M, FitzGerald M. Exposure to furry pets and
the risk of asthma and allergic rhinitis: a meta-analysis. Allergy 2008. 63(7):857-865